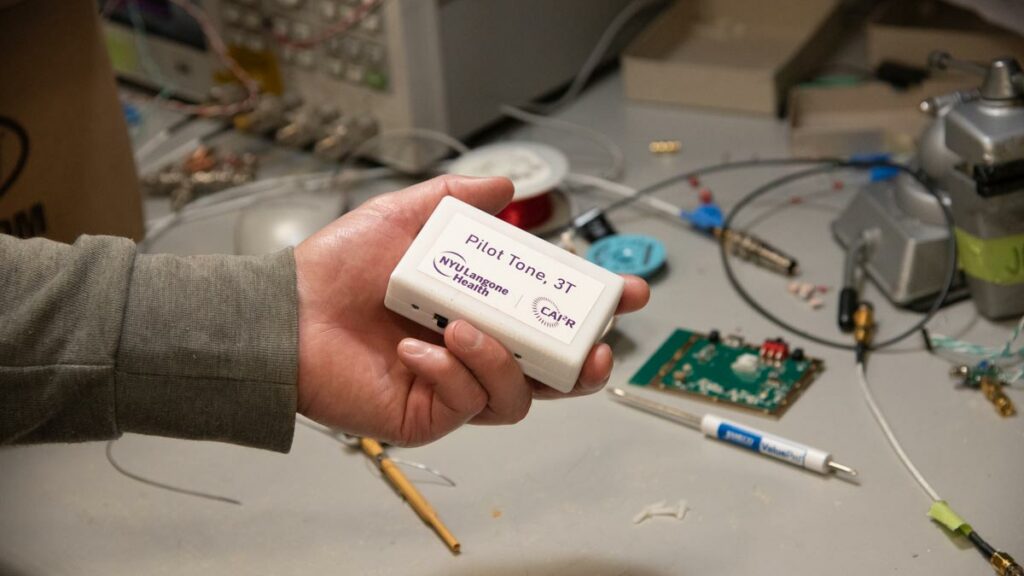
On a Thursday afternoon in mid October, Jan Paška, PhD, research scientist with the Center for Advanced Imaging Innovation and Research at NYU Langone Health, stood at his workbench in the RF laboratory as he slid a bubble-wrapped object, about the size of a bar of soap, into a cardboard envelope addressed to Boston Children’s Hospital. The item, a 3-Tesla wireless pilot tone transmitter, was the second headed to Boston Children’s and the sixteenth dispatched by Dr. Paška to research teams trying to solve one of the most pervasive challenges in MRI: respiratory motion.
“We recently got our IRB approval to use the pilot tone in clinical patient scans—that’s why we asked Jan if we could have a second [device],” said Cemre Ariyurek, PhD, postdoctoral fellow at Boston Children’s. Dr. Ariyurek and colleagues are working on better diagnostic tools for a kidney condition called hydronephrosis, in which urine accumulates in the organ instead of draining away.
“We want to measure the glomerular filtration rate of the kidney to detect whether there’s an obstruction and to decide which patients should go into surgery,” said Dr. Ariyurek, referring to a metric of the organ’s function. “Dynamic contrast enhanced MRI has been widely used to determine filtration rate, but image quality may be deprecated because of motion,” she said. Because contrast injections cannot be immediately repeated, a scan marred by motion means moving on with incomplete data or calling patients back to schedule another MRI. “If you miss it, you miss it.”
Although we may not think of abdominal organs as mobile, they change position and shape as they’re pushed and pulled by the rise and fall of the diaphragm as it inflates and deflates the lungs. These displacements, like any motion, cause loss of definition in MR data and images. Pediatric patients, who tend to have a hard time keeping still and controlling their breath, present an even greater challenge than do most adults. To prevent errant movements of anxious, inattentive, or otherwise noncompliant children, doctors often resort to sedation—but even sedated patients breathe. “Glomerular filtration rate estimated from those images might be inaccurate,” said Dr. Ariyurek.
The pilot tone transmitter is a standalone wireless device that emits a radio signal at a constant frequency, set at the margin of an MRI acquisition. When a patient moves, the RF coils gathering data inside the scanner record changes in the signal’s amplitude, turning the pilot tone into a running motion reference, a bit like metadata attached to each frame in a video.
The concept was invented in 2014 by Peter Speier, PhD, an engineer at Siemens Healthcare. At the time, Dr. Speier was experimenting with respiratory navigation based on noise. Disappointed by the results, he had the idea to substitute noise with a coherent signal—a pilot tone.
In 2015, as Siemens was about to report its preliminary findings at an annual meeting of the European Society for Magnetic Resonance in Medicine and Biology, Dr. Speier approached Fernando Boada, PhD, then co-director of the Center for Advanced Imaging Innovation and Research, thinking that Dr. Boada’s PET/MR studies may serve as fertile ground for probing the limitations and practical potential of the pilot tone principle.
“They basically asked me, do you want to take a look at that?” said Dr. Boada, who is now the associate chair for basic science translational research at Stanford University. The concept’s simplicity appealed to him: the pilot tone would not require strapping anything to a patient or synchronizing external data with the MRI signal.
Ryan Brown, PhD, associate professor of radiology at NYU Langone, assembled the team’s first transmitter, a wired setup that consisted of an antenna hooked up to a signal generator. “Because it’s so simple . . . we were up and running the first time we tried it,” he said.
The group’s subsequent research, performed in collaboration with Siemens, led to presentations at the annual meetings of the International Society for Magnetic Resonance in Medicine in 2016, 2017, and 2018, seeding interest in the research community. In early 2020, the journal Investigative Radiology published peer reviewed findings that the method “provides reliable respiratory motion tracking during arbitrary imaging sequences.”
Meanwhile, Siemens engineer Jan Bollenbeck developed a wireless 1.5 Tesla version of the transmitter, eliminating the need for the bulky signal generator, and NYU Langone’s Dr. Paška adapted the new design to applications at 3 Tesla, a magnetic field strength favored among MRI scientists.

Around that time, Eddy Solomon, PhD, then postdoctoral fellow at NYU Langone, made it his mission to characterize the wireless 3T pilot tone. “I took the device from Jan Paška, and I started really trying to understand how to work with this,” he said. The team experimented with the transmitter’s location, orientation, different types of motion, and a variety of RF pulse sequences. “Another thing is that we had to develop a pilot tone detection algorithm to be able to extract the signal modulation from k-space and make sure it stays clean and is not affected by the extraction,” said Dr. Solomon, now an instructor at Weill Cornell Medical College.
One fruit of these explorations was a sort of how-to paper that appeared in late 2020. Another was computer code for working with the 3T pilot tone signal. In addition, Siemens allowed the Center for Advanced Imaging Innovation and Research to share the 3T pilot tone transmitters. Taken together, these resources added up to something of a start-up package for researchers interested in exploring the new technology. “It’s not exactly plug and play, but it’s not far from that,” said Dr. Solomon.
Part of the appeal lies in the method’s technical flexibility. “MRI can be set up to have motion navigators built into the [RF pulse] sequence, but that immediately makes my MRI sequence very specialized,” said Dr. Brown. “In practice, you want to be able to apply any sequence you like.”
The Boston Children’s team in pursuit of more accurate MRI measurements of kidney filtration rate first sought to correct the organs’ motion by adapting FID navigators, a technique used to deduce underlying movement from differences in signal received by individual elements in an RF coil array. Although the navigators did reduce blur in images, it became apparent that the approach would require complex modifications before it could be used to gauge kidney function. “We realized that FID navigators are affected by the contrast, so it’s hard to distinguish MR signal proceeding from the contrast and [signal caused by] motion,” said Dr. Ariyurek. The team began wondering about alternatives.
“We started to build this idea whether we may apply the pilot tone,” said Tess Wallace, PhD, instructor at Boston Children’s who investigates motion correction in MRI. She had heard about the technology at the annual meetings of the International Society for Magnetic Resonance in Medicine, where both Siemens and NYU Langone researchers presented on the subject. “We came back one year and started doing a bit of a literature search,” which brought them to a 3T Pilot Tone resource page with information about getting transmitters for free. “We thought, that’s a bit too good to be true, but let’s email and find out,” she said. “And then NYU sent the device.”
Offering access to leading-edge research tools is part of the mandate of the Center for Advanced Imaging Innovation and Research as per its founding grant from the National Institutes of Health. But the wireless 3T pilot tone transmitter is the first physical device to reach the Center’s broadest dissemination tier, where anyone can request and download resources.
“Research hardware has been notoriously difficult to share,” said Dr. Brown. For example, the construction of novel RF coils—second only to scanners in importance for MRI research—is widely considered something of an art and requires engineers to iteratively test and tune coil prototypes in search of optimal arrangements of electronic elements with respect to the intended imaging application, anatomy of interest, and MRI system. “It’s labor intensive,” said Dr. Brown.
Although the 3T pilot tone transmitter is not an MRI coil, the device’s rapid dissemination shows how continuing miniaturization of electronics, increasing flexibility of supply chains, and falling costs are beginning to alter the calculus for research hardware.
The printed circuit board (PCB), a component at the heart of electronic devices, is a case in point. Until relatively recently academic scientists had to build application-specific PCBs in-house. Purchasing industrially made equivalents required ordering industrial quantities—and paying prices—that rarely made sense for research purposes. Today, overseas PCB houses manufacture custom boards in small batches at low cost. Dr. Paška, who adapted PCB design for the 3T pilot tone transmitter, has the components made in China and shipped to NYU Langone’s RF lab in boxes of just 10 units.

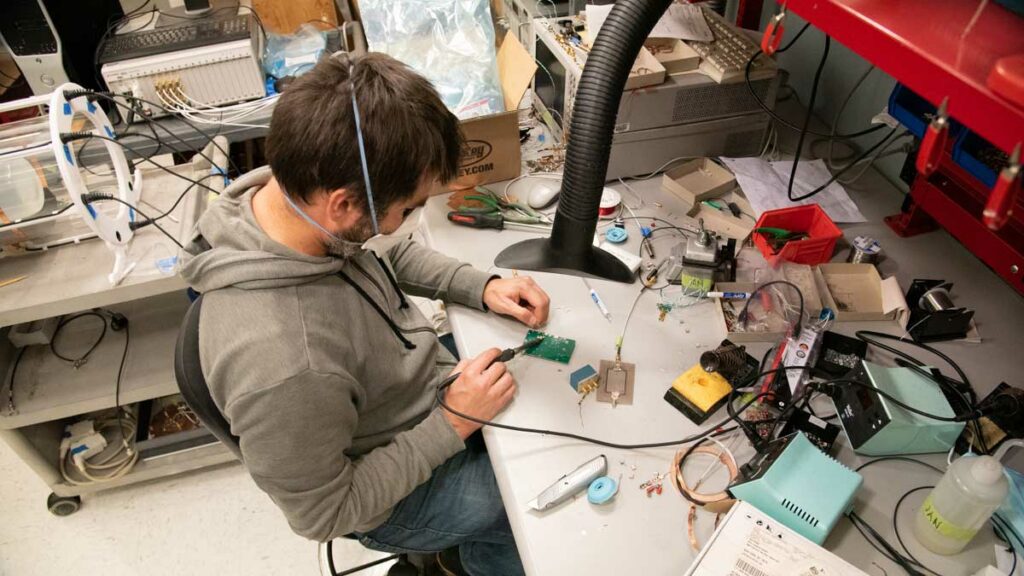
To assemble a transmitter, Dr. Paška unseals a PCB, solders on a power switch, attaches a battery, and adds a copper-tape RF shield. Then he places the PCB inside a plastic case 3D printed in the lab. He tests the power switch and the LEDs, disconnects the built-in antenna, and hooks up the transmitter to a spectrum analyzer. If the analyzer shows a reading of -20 dBm at the pilot tone frequency, Dr. Paška reconnects the antenna, closes the housing, and takes the measurement again—this time with an external pick-up loop. If the second reading looks good, he bundles the transmitter with a USB cable (for charging) and a 1.5-millimeter flathead screwdriver (for amplitude adjustments), and ships the bundle out. The whole process, he estimates, takes about four hours.
More than a dozen research groups are now experimenting with these transmitters. At Brigham and Women’s Hospital in Boston, scientists are exploring a combination of the 3T pilot tone and ultrasound sensors for motion-correcting MRI and PET/CT data. A team at Massachusetts General Hospital is researching whether PET/MR informed by the pilot tone can characterize the progression of idiopathic pulmonary fibrosis and show patients’ response to anti-fibrotic therapy. Another team at the same institution is looking into ways to keep track of head movement during PET/MR neuroimaging exams. At Lausanne University Hospital in Switzerland, scientists are incorporating the pilot tone into an imaging study of heart failure. More investigations are under way in the U.S., Canada, France, the Netherlands, and Poland.
The popularity is driven by an unsolved and prevalent need in MRI. “The pilot tone happens to address challenges with motion, which occurs in every scan,” said Dr. Brown. “Even in organs we might not expect, like the brain or the prostate, that we tend to think of as stationary.”

The pilot tone approach exemplifies a larger trend in which scientists look to accessorize MRI scanners in an attempt to circumvent the systems’ limits. Inspired by the proliferation of sensors in the realm of everyday life—LIDARs guiding self-navigating vehicles, time-of-flight cameras “face-unlocking” smartphones, and wearable multi-sensor arrays tracking personal vitals—medical imaging researchers have begun to imagine similarly informative contributions to MRI.
Even so, the use of external sensors can cause image artifacts and pose synchronization issues, forcing scientists to figure out how to mitigate interference and align data from independent sources, each with its own sense of time. “It’s actually not super trivial,” said Dr. Brown, who has also investigated motion tracking in MRI with time-of-flight cameras, which sense depth by clocking the bounce-back of emitted light.
Among the many sensing strategies attracting attention, the pilot tone stands out as a native in the context of electromagnetic fields, radiofrequency pulses, and k-space sampling. The technology’s early dissemination suggests that the promise of scanner “sensorization” becomes more cogent when the sensors themselves speak the language of MRI.
“Someone who picks up the pilot tone … there’s a lot of directions you can take this,” said Dr. Solomon. And that’s exactly what the pilot tone recipients at Boston Children’s and elsewhere are doing as they use the devices to overcome challenges posed by respiratory motion. Dr. Brown said that he’s contemplating setting up a user group. “Hopefully we can learn from each other,” he said.
This story was published on December 7, 2022, and updated that day to clarify the pilot tone description in the fifth paragraph.
Related Resource
A compact, stand-alone device for tracking and correcting patient motion in MRI exams.
Related Story
RF coil engineers at NYU Langone Health needed an interface compatible with a new industry standard, so they built one. Now NYU Langone is shipping the devices to other advanced MRI labs.


