Yongxian Qian, PhD, is an assistant professor of radiology at NYU Grossman School of Medicine and scientist with the Center for Advanced Imaging Innovation and Research at NYU Langone Health. His work ranges across several technical aspects of magnetic resonance imaging, including pulse sequence design, image reconstruction, and coil development. Dr. Qian’s investigations cover many areas of clinical application, including knee osteoarthritis, brain cancer, traumatic brain injury, and Alzheimer’s disease. In recent years, he has taken a growing interest in the implications of quantum technologies for research and development in MRI. Our conversation was edited for clarity and length.
Your career in MRI research has spanned more than twenty years and roamed through many areas in the field. But before your PhD, you had earned a BS in physics and an MS in geophysics. How did you find your way to MRI?
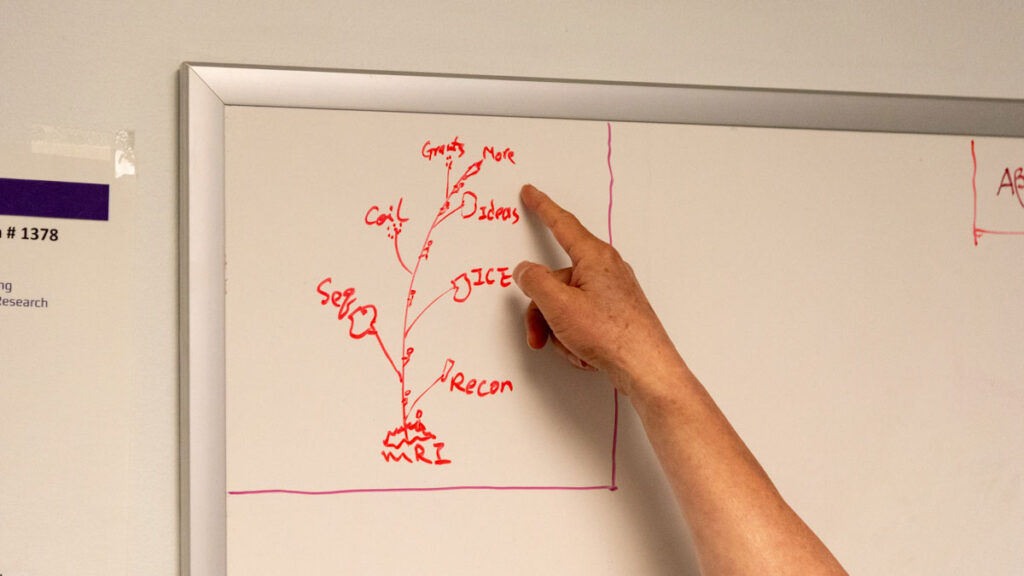
Actually, on my office white board there is drawing of my MRI career tree, and it starts from imaging reconstruction. This was a logical choice when I was looking for a research topic for my PhD thesis in biomedical engineering. My master’s was in seismic data processing for oil and gas exploration, and I thought it would lend itself well to things like MRI. My PhD advisor specialized in cardiac electrical signal processing, not MRI reconstruction, so I had to convince him that with my experience in seismic imaging of the Earth and my background in physics I could go in that direction.
Reconstruction did not require scanning, only data. I reached out to the MRI research community, and the German Cancer Research Center [DKFZ] provided me raw imaging data acquired with spiral trajectories. I worked on reconstructing those with an algorithm I developed.
You did your doctorate at the Huazhong University of Science and Technology in China. So, you not only proposed a dissertation subject outside of your advisors’ area of expertise but also obtained data for your research from another country?
That’s correct. I developed an algorithm for MRI reconstruction and published two papers in Magnetic Resonance in Medicine, a top journal in the field. That’s how I got a PhD in just three years: after those papers, my university was like, well, you’re ready.
What was it about MRI reconstruction that made you want to pursue it?
Reconstruction was an opportunity to translate my career from imaging the Earth to imaging the human body. I have a strong background in mathematics and physics, but I liked the idea of solving challenges that would have clinical applications. Fast imaging, specifically spiral imaging, had just come out—that was before EPI technologies became popular—and I thought I could do some mathematical work on non-Cartesian imaging. That’s how I started in MRI.
Then I moved on to sequence programming. It was tough. To develop new pulse sequences, you have to understand the hardware and the software of the system really well and put your new ideas in that framework. It takes a long time to learn that.
You mean that one has to understand the proprietary languages and the specifics of a particular manufacturer’s platforms.
Yes, and that’s also true for online reconstruction, which is what you do when want the image to come out immediately after acquisition. For example, on Siemens systems there’s something called image calculation environment, or ICE, and that’s even more complex than sequence development.
You completed postdoctoral training at the University of Pittsburgh Medical Center. How did you choose that destination?
Actually, I had applied for another position in New Mexico. They required a reference letter, and I asked someone at Pittsburgh to write it. That advisor said, ‘why do you want to go to New Mexico? Come join us here.’ UPMC had dedicated MRI scanners for research, so I thought, why not?
Who did you work with at UPMC?
My first PI was Yi Wang. Under his direction, I continued my work on image recon and learning pulse-sequence programming. Two years later, my P.I. wanted to move to New York City, but I preferred to stay in Pittsburgh. So I switched to my second P.I., Fernando Boada.
Around that time, you also begin to look at particular MRI applications—as opposed to reconstruction—for example, in knee cartilage.
Yes, Fernando’s lab had a collaboration with researchers who needed MRI physicists to support an NIH-funded project to study osteoarthritis. I developed a spiral ultra-short echo time sequence for knee MRI—first of that kind, and we got a patent for it. Cartilage has a very short T2 relaxation time, so you need short and even ultra-short echo times to get signal. And you also need speed, which is where spiral trajectories help.
That collaboration led to award-winning research. [It was recognized with the Kappa Delta Elizabeth Winston Lanier Award at the 2019 annual meeting of the American Academy of Orthopaedic Surgeons]. The research team defined a new stage between ACL injury and osteoarthritis called pre-osteoarthritis, an interval when the damage that can lead to OA may still be reversible.
That’s the concept proposed by Constance Chu, the principal investigator of that project. There’s currently no cure for osteoarthritis. You can try to delay the progression, but there’s no way to reverse it. In order to prevent OA, you have to identify it before clinical diagnosis, and to do that you need a technology to detect it.
Let’s talk about sodium MRI, which has been one of the themes in your research. How did you first get involved in sodium imaging?
That started with Fernando. Sodium MRI was a major part of his research when we worked together in Pittsburgh. He developed trajectories called twisted projection imaging, or TPI, to optimize the signal-to-noise ratio, because sodium has very low SNR compared with the regular proton images. I worked on programming for the sequences when we switched from GE to Siemens systems, and I brought my experience with spiral sequences.
Sodium imaging is part of an NIH-supported project you lead that explores the role of cerebrospinal fluid clearance mechanisms in aging and Alzheimer’s. Can you talk about that investigation?
We’re working to see how the efficiency of CSF clearance changes in the normal aging population and how it’s altered in Alzheimer’s patients. We look at CSF production, flow inside the brain, and drainage out of the brain.
How is CSF clearance related to the glymphatic system, known for removing waste from the central nervous system?
CSF clearance is a big concept, and the glymphatic system is just one of multiple pathways to do the clearance. In our project, we follow the CSF bulk flow. We are not focused on the perivascular space, through which the glymphatic system is hypothesized to work.
Is the CSF clearance pathway you’re looking at related to sleep?
That’s a good question. The first aim of our project is to see how the CSF clearance properties—production, flow, and drainage—change with age in the cognitively normal population. The second aim is to see how sleep affects these properties. And our third aim is to see whether there are differences between the healthy aging people and people with Alzheimer’s.
In order to study this, do you have to image people while they’re asleep?
Yes, we ask our study subjects to sleep inside the magnet for an hour and a half.
MRI can be noisy. Is it challenging for people to drift into sleep inside a scanner?
Most people can fall asleep. We use MRI-compatible electroencephalography [EEG] to monitor sleep state. Sleep has four stages: N1, N2, N3, and REM. Some people can get to N3, that’s deep sleep. Most only get to N1 or N2. We match EEG staging with our sodium MRI data to see what the CSF flow inside the brain is at different sleep stages.
In studies of animals, researchers found that during sleep CSF clearance efficiency doubled. In mice, the extracellular space is increased by 60 percent during sleep and that allows the CSF to go through, facilitating the clearing of amyloid beta protein out of the brain and increasing clearance rate by 100 percent. But we don’t know whether that beneficial impact also happens in humans because we haven’t had the technology to see that. But now, in our group, we have it.
And what are you learning?
So far, we know that during sleep extracellular space in the brain is changing. We use sodium MRI to detect and quantify extracellular space, and we expected the sodium signal to increase, which would match findings in animal studies. But our preliminary data analysis indicates that the space is decreased. We’re working on statistical analyses that can help explain these results and designing additional, postmortem studies that may help us understand these findings.
Can you say briefly why sodium is so important in the brain?
For neurons, for example, and their electrical activity—what we call the firing of the neurons. In a healthy brain, the concentration of sodium ions outside the cell is about ten times higher than inside. This gradient is actively maintained by the sodium-potassium pump. But in some pathological alterations, intracellular sodium is increased. This can disrupt the normal function of neurons and their communications, which is then reflected in cognition.
You recently led a paper describing a new method of separating two types of sodium in the brain. The separation method you and colleagues have developed is significantly more accurate than prior techniques. Can you talk about that study and how it relates to the other questions you’re asking in your research?
We’ve worked on that for more than ten years, actually, to see how to make sodium images more sensitive to cellular-level changes. Right now, most people focus on total sodium, but sodium concentrations outside of the cells are higher, so they have high signal, which overshadows the changes inside cells. We try to remove that kind of signal and make sodium imaging more sensitive to the changes inside cells.
What are the potential benefits of being able to do this kind of separation?
One potential benefit is to aid with early diagnosis in conditions like Alzheimer’s by helping detect changes inside the cells before the appearance of clinical symptoms. And with early diagnosis some interventions may be more effective.
There’s also potential for monitoring response to treatment. Right now, treatments for Alzheimer’s disease have significant side effects. Close monitoring and follow-up scans could help track how the patient is responding to the treatment on the cellular level rather than waiting for the cellular conditions to show up as symptoms.
And another potential benefit is for patients with cancerous tumors. Cancers respond differently to different therapies, and there are a lot of treatment options, so care plans tend to change based on the cancer’s response. Right now, it can take a couple of months before that response can be known.
And the current standard measure of that response is tumor size, correct?
Yes, tumor volume—is the tumor shrinking? But we can apply sodium MRI to detect cellular-level change in the tumor tissue in just a couple of weeks or even one week following the start of treatment. For brain tumors, gliomas, the average survival is just 18 months, so time is very precious for patients. If one kind of treatment is not effective, the care team has to switch to another option. These applications are in research stage, but we hope to eventually get them to the clinic.
What are some of the main challenges here?
The major issue to get sodium imaging to clinical applications is signal-to-noise ratio. It’s still a thousand times lower than for proton images—not high enough for clinical use. We’re trying to use quantum technologies to increase it.
When you say quantum technologies, what do you mean?
By quantum technologies, I mean four topics: quantum sensing, quantum computing, quantum simulation, and quantum communication.
With quantum computing and quantum sensing, we’re developing MRI techniques that can detect neuronal electric activity directly, without contrast injections. These topics can also be applied to sodium imaging and to imaging macromolecules because MR signal originates with nuclear spins, and each spin is a quantum bit, or qubit.
For example, sodium nuclear spins have four energy levels, so they’re equivalent to two qubits. We can use quantum computing algorithms to design pulse sequences that initialize or manipulate the quantum state of sodium nuclear spins to some excited state, amplifying the sodium signal.
We also plan to investigate quantum computing for [hydrogen] proton spins based on amyloid beta proteins, which are linked to Alzheimer’s. We try to identify the proteins and see how many qubits they can produce based on their proton nuclear spins. Proteins are macromolecules, so they have connections between proton nuclei equivalent to multiple qubits. Once we figure out that part, we can do quantum computing to design sequences that amplify the MR signal specifically from the Amyloid beta protein and do molecular MRI without contrast injections.
In other words, quantum computing might help make MRI specific to molecules of interest. What about quantum simulation?
Quantum simulations are needed to simulate the spin states of molecules or protein in order to come up with the manipulations of those states. The manipulations themselves are MRI pulse sequences, but we need the simulations in order to design the sequences in a way that targets only the molecules we’re interested in and not others.
And you also mentioned quantum communication—what is that?
Actually, much development in quantum computing is driven by quantum communication, because many sectors—including defense, finance or healthcare—need to securely exchange information, and quantum communication is so far the best solution. Some of the algorithms or technologies developed in quantum computing could help us identify how molecules or proteins communicate between their spins or learn how to make them communicate. But right now, our research is just focused on the first three areas: quantum sensing, quantum computing, and quantum simulations.
You have for a long time now led a journal club at our research center dedicated to quantum computing advances. At every meeting, you and colleagues discuss new publications in the field and talk about potential implications for MRI. What accounts for your special interest in quantum technologies?
During the pandemic, when everyone worked remotely, I had a lot of time to read academic literature. By chance, when I was going through an issue of Nature, I read a paper about quantum computing. It was very interesting to me, because my background is in physics and I’m good at quantum mechanics. I saw that the authors used nuclear magnetic resonance to confirm a quantum computing concept, and I realized that there are close connections between MRI and quantum computing. Most people use quantum computing to accelerate calculation, like electromagnetic simulations. But I saw another potential application, directly to MRI.
I’m currently the guest editor for a special collection on quantum technologies for healthcare for Scientific Reports—it’s a Nature Portfolio journal that covers the four major areas I mentioned.
How far would you say we are from this vision of using quantum techniques to make MRI specific to macromolecules based on their nuclear spin characteristics?
We have a lot of work to do to develop imaging technologies based on quantum computing concepts. I think that’s the next ten to twenty years, and I intend to stay in this area. That’s my vision for the next generation of imaging: MRI for molecules.
Related Story
NYU Langone scientists propose MRI sodium separation method with potential to inform research on ion imbalances in neurological conditions.