RF coil engineers at NYU Langone Health needed an interface compatible with a new industry standard, so they built one. Now NYU Langone is shipping the devices to other advanced MRI labs.
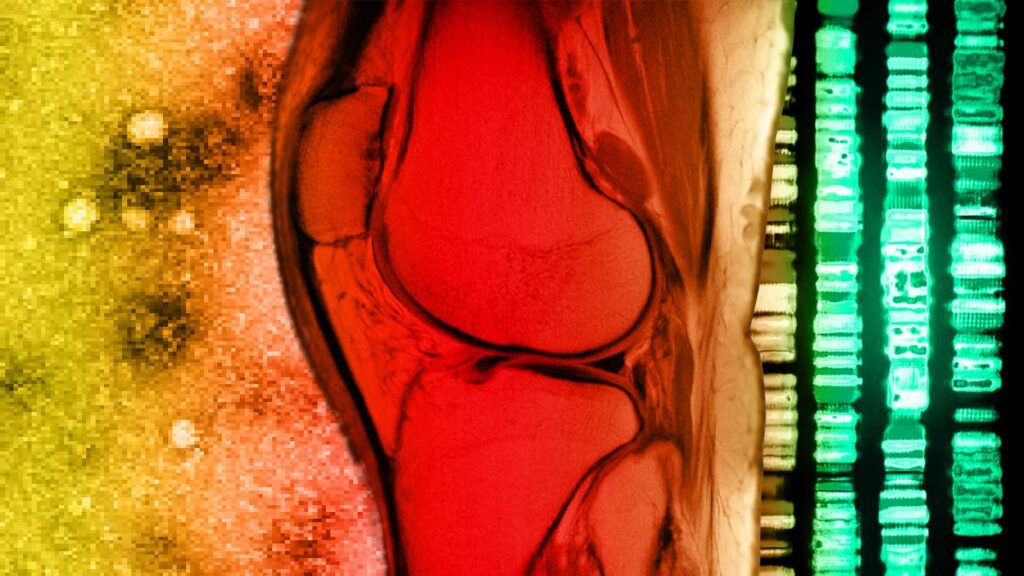
PTOA is affecting more people earlier but medicine cannot predict who. The National Institute of Arthritis and Musculoskeletal and Skin Diseases is funding NYU Grossman School of Medicine to create an advance warning.
How a moonshot effort to build an open-source MRI scanner from scratch in less than a week played out, and what it means for imaging research at large.
In a return from a pandemic hiatus, the i2i Workshop encouraged a broad and varied look at what imaging is and where it’s headed.
Ilias Giannakopoulos, postdoctoral fellow in MRI, talks about how electromagnetic waves interact with the body, why matrix compression matters, and where he finds inspiration.
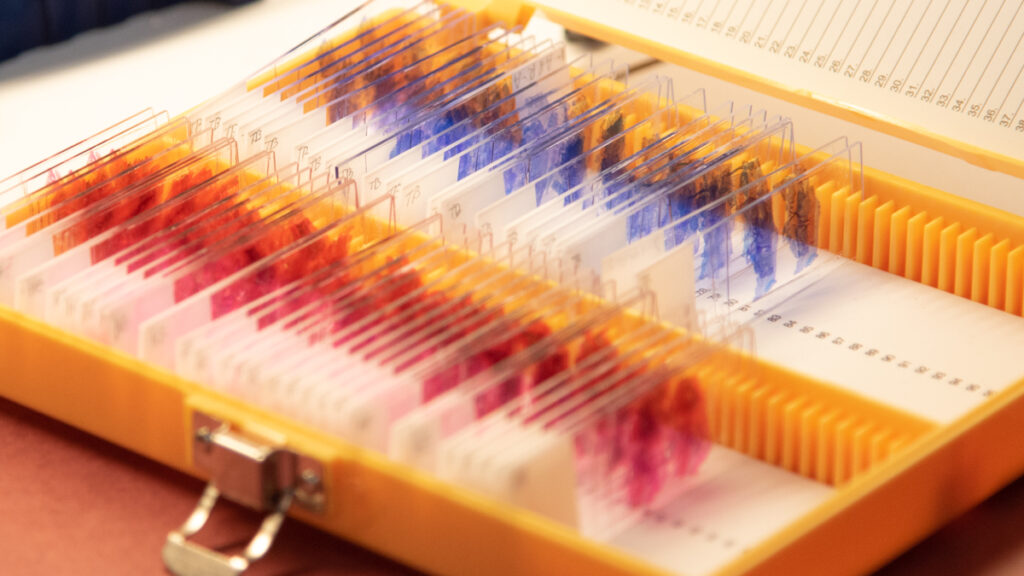
A team of scientists is using a battery of imaging methods to visualize cells, tissues, and joints in a quest for early noninvasive imaging biomarkers of PTOA.
Radhika Tibrewala, graduate student in biomedical imaging, talks about the new fastMRI prostate dataset, deep learning in MRI, and how she started a PhD remotely in 2020.
Wafer-like materials studded with nanofabricated protrusions enable researchers to direct light and contemplate new optical devices.
Li Feng, developer of fast MRI techniques, talks about going beyond speed, his path to academia, and the rewards of persistence.
The Society for Cardiovascular Magnetic Resonance has bestowed its highest honor on Leon Axel, radiologist, scientist, and longtime developer of MRI methods to better understand the heart.